Physiology Review
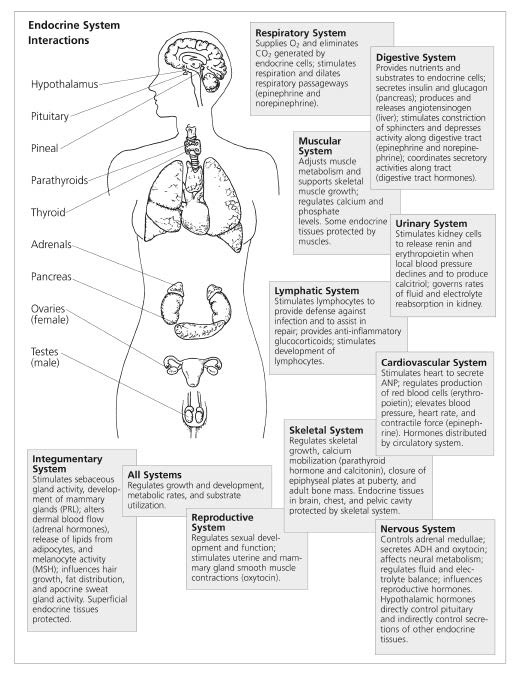
The endocrine system involves all the organs and their supporting tissues that are involved in secreting hormones into their respective capillaries that eventually travel through the blood and cause specific effects on target tissues of the body. Hormones are chemical agents that cause a specific effect on target tissues outside the initial place they are produced. Hormones work along with the nervous system to integrate and harmonize various physiological functions, such as growth and reproduction, related activity and homeostasis (a tendency to stability in the normal body states or internal environment).
Endocrine Tissues
Endocrine tissues or glands are distinguished from exocrine glands in that they have no ducts. Some endocrine secretory cells are located in non-endocrine organs (such as the enteroendocrine glands of the gastrointestinal tract), interstitial cells of the testes, secretory neurons in the brain (such as the hypothalamus), or may exist as microscopic islands (such as the beta cells of the Langerhans of the pancreas). The remaining endocrine tissues exist as an entity, namely the pituitary gland, pineal gland, thyroid glands, parathyroid glands, thymus, adrenal glands, ovaries, and testes.
Other Hormone-Secreting Organs
Endocrine activity also involves certain organs that have crucial functions outside this role.
Kidneys: For example, the kidney not only secretes renin involved in blood pressure, but also erythropoietin that stimulates red blood cell corpuscles.
GI Tract: The gastrointestinal tract is involved in production of hormones regulating digestion.
Placenta: The placenta secretes human chorionic gonadotropin (HCG), estrogen, progesterone, lactogen, and growth-stimulating hormone.
Heart: The heart secretes atrial natriuretic peptide (ANP) involved in sodium excretion and inhibits smooth muscle contraction.
Hypothalamus
Intimately involved with the endocrine system is the hypothalamus, controlled by secretory neurons that control the release of hypophyseal hormones from the pituitary gland. These include follicle-stimulating hormone (FSH), leuteinizing hormone (LH), thyroidstimulating hormone (TSH), adrenocorticotropic hormone (ACTH), growth hormone (GH), prolactin, oxytocin, and antidiuretic hormone (ADH). These hormones tell their respective organs to produce estrogen, progesterone, testosterone, thyroxin, and adrenal cortical hormones.
Receptors
Endocrine hormones typically act to control intracellular functions by first combining with hormone receptors on the surfaces of cells or inside the cells. Binding of the hormone with the receptor turns on a cascade of reactions within the cell to accomplish a particular goal. These hormone receptors are very large proteins, and each cell may have in the order of 2,000 to over 100,000 hormone receptors, depending on the cell’s function. Receptors are understandably highly specific for a single hormone. This allows one hormone to act on a particular target tissue with minimal cross reactivity.
Amazingly, the number of receptors in a target cell is in constant flux. For example, the binding of a hormone with its corresponding receptor causes the number of receptors to change. In “down-regulation” the number of receptors is reduced, causing a decreased responsivesness to the hormone. In “upregulation,” the number of receptors is increased with a corresponding increase in hormone sensitivity. This phenomenon is responsible for many of the clinical effects seen with medical intervention, including some of the tolerance that develops to longer-term pharmaceutical treatments (and thus the need to adjust dosages) and the drug withdrawal symptoms commonly experienced when a drug or hormone treatment is discontinued. It may also help us to explain how therapies that balance the endocrine system can lead to long-term changes and bring patients to a new plateau in their wellness.
Feedback Mechanisms
Control of hormone secretions is accomplished by an internal control system. In most instances, a feedback mechanism is employed. The majority of feedback loops work as a negative feedback. In negative feedback, the endocrine gland has a natural tendency to oversecrete its hormone. The hormone then stimulates the target tissue to perform a function. Thus, the important factor is not the rate of secretion of the hormone but the rate that the target function is performed.
When the target organ’s activity rises to an appropriate level, feedback is released to the endocrine gland to slow further secretion of the hormone. For example, the pituitary gland (endocrine gland) secretes thyroid-stimulating hormone, which acts on the target organ, the thyroid gland, to stimulate production of the thyroid hormones T3 and T4. The pituitary then monitors the circulating levels of thyroid hormones. When these levels are deemed by the pituitary to have reached appropriate levels, the release of TSH by the pituitary is curtailed. If the target organ (in this case the thyroid gland) were not to be able to produce adequate amounts of thyroid hormones, a healthy pituitary would secrete more and more TSH until the thyroid gland responded.
| Endocrine Tissue | Hormone |
|---|---|
| Anterior Pituitary | Growth Hormone (GH)
Adrenocorticotropin Hormone (ACTH) Thyroid-Stimulating Hormone (TSH) Follicle-Stimulating Hormone (FSH) Luteinizing Hormone (LH) Prolactin |
| Posterior Pituitary | Antidiuretic Hormone (ADH) Oxytocin |
| Pineal | Melatonin |
| Thyroid Gland | Thyroxine (T-4), Triiodothyronine (T-3) Calcitonin |
| Parathyroid Glands | Parathormone (PTH) |
| Adrenal Glands (medulla) | Adrenaline and Noradrenaline |
| Adrenal Glands (cortex) | Cortisol Aldosterone DHEA |
| Pancreas | Insulin Glucagon |
| Ovaries | Estrogens Progesterone |
| Testes | Testosterone |
| Hypothalamus
Although not considered an endocrine gland, the hypothalamus exerts control over the pituitary via neuro-hormones. |
Corticotropin-Releasing Hormone (CRH)
Growth Hormone-Releasing Hormone Growth Hormone-Inhibiting Hormone Gonadotropin-Releasing Hormone (GnRH) Thyrotropin- Releasing Hormone (TRH) Prolactin Inhibiting Factor (Dopamine) |
| Site of Action | Action |
|---|---|
| Most cells of the body | Stimulates cell growth |
| Adrenal Glands (cortex) | Stimulates adrenal cortex to release cortisol and aldosterone |
| Thyroid Gland | Causes thyroid to secrete thyroid hormones |
| Ovary/Testes | Promotes growth of follicles within the ovary (female), sperm formation (male) |
| Ovary/Testes | Stimulates estrogen/progesterone release (female), testosterone (male) |
| Breast tissue | Encourages breast development, milk production in pregnancy |
| Kidneys, blood vessels Uterus/Breast tissue |
Causes kidneys to retain water, increases blood pressure Induces contractions during labor, milk expulsion |
| Brain, immune system | Governs sleep/wake cycle |
| Most cells of the body Bone cells |
Increases metabolism, chemical reactions Increases calcium deposition |
| Gut, kidney, bone | Increases calcium in the blood |
| Many cells and tissues | Initiates fight-or-flight response |
| Many cells and tissues Kidneys, sweat glands Immune system, brain |
Stress response affects metabolism, immune system, blood vessels Promotes sodium/water retention, increases potassium loss Precursor to androgens, promotes immune and mood balance |
| Most cells of the body Liver, fat, muscle |
Promotes entry of sugar into cells, fat deposition Increases glucose production and release into the blood |
| Sex organs, uterus, bone, brain Sex organs, uterus, bone, brain |
Involved in sexual development (female), menstruation, builds uterine tissue, bone metabolism Involved in sexual development (female), menstruation, uterine secretion, pregnancy |
| Sex organs, brain | Involved in sexual development (male), libido, muscle development |
| Anterior Pituitary | Stimulates release of ACTH
Stimulates release of GH Inhibits release of GH Stimulates release of LH and FSH Stimulates release of TSH Inhibits release of Prolactin |
Endocrine Disorders
Endocrine disorders can be attributed to any malfunction of endocrine tissue. There are many ways that an endocrine system can go astray. The endocrine tissues can either secrete too much or too little hormone, or the peripheral tissues can’t process the hormones. The causes can be quite varied — infections, tumors, trauma, and lifestyle factors. These endogenous factors can disrupt the endocrine system. Exogenous factors, such as chemicals in the environment, can also cause a host of complications in the endocrine system. These endocrine disrupters are found in high levels in non-organic foods cultivated with pesticides, in our water supply, and in the air we breath.
Pituitary Disorders
These disorders include pituitary insufficiency resulting in the failure of the pituitary to release or produce adequate amounts of growth hormone, prolactin, corticotrophin, thyrotropin, leuteinizing hormone, or follicle-stimulating hormone. Excessive hormone production can also occur, caused by growth-hormone- secreting pituitary tumors and glycoproteinsecreting pituitary tumors.
Pineal Disorders
Pineal disorders as recognized by conventional medicine are quite rare. They consist of tumors that are benign (pinealocytoma) and aggressive pineal cell tumors (pineoblastoma, pineal germinoma, pineal teratomas). Pineal cysts are most often not treated, unless they are large enough to cause hydrocephalus or visual symptoms.
Although not recognized conventionally, melatonin deficiency and excess is a relatively common condition that can be the root of many symptoms. The pineal gland is responsible for melatonin production. If it is underactive in producing melatonin, this can cause various symptoms, such as insomnia and stress. If it is overactive, the result can be seasonal affective disorder (SAD).
Blood Sugar Metabolism Disorders
Disorders of blood sugar metabolism involve problems with either the pancreas producing too little or too much insulin, the insulin receptor sites becoming deficient, or decreased function of the adrenal glands or liver. The most common blood sugar disorders are diabetes Type I, diabetes Type II, and hypoglycemia. The secondary complications to diabetes range from increased cardiovascular risk to end-stage renal disease.
Lipids Metabolism Disorders
Disorders of lipid metabolism involve problems associated with either overly high or overly low levels of fats in the body. The most common disorder of lipid metabolism in the modern affluent world is high levels of lipids (cholesterol and triglycerides) due to excessive eating of high-fat foods and low levels of physical activity. Although much more rare, some people suffer from excessively low levels of lipids usually due to malabsorption of fats due to digestive disorders.
Thyroid Metabolism Disorders
Thyroid disorders are usually related to hyperfunction or hypofunction of the thyroid gland, resulting in hyperthyroidism or hypothyroidism. Secondary complications to hypothyroid are weight gain, fatigue, and cardiac complications; secondary complications to hyperthyroid are atrial fibrillation, weight loss, and anxiety. Chronic fatigue syndrome, fibromyalgia, and Wilsons temperature syndrome are disorders suspected of being related to decreased peripheral thyroid hormone conversion or thyroid resistance.
The parathyroid glands are found next to the thyroid, and when over activated, lead to excessive levels of calcium in the body, resulting in symptoms ranging from hypertension and headache to depression and kidney disease.
Adrenal Metabolism Disorders
Adrenal disorders, like most endocrine disorders, are usually associated with hyperfunction or hypofunction. Adrenal hyperfunction can lead to hyperaldosteronism, resulting in hypertension, and adrenal insufficiency, resulting in severe fatigue. Naturopathic medicine recognizes adrenal insufficiency in a much more wider diagnostic parameter than conventional medicine.
Reproductive Hormone Disorders
Reproductive endocrinology is associated with any reproductive hormone level change. Common conditions include impotence, hirsutism, and infertility. It also covers healthy and normal changes of hormone levels associated with changes of maturation, such as puberty and menopause.
Endocrine Disruptors
Besides endocrine disorders caused by the internal environment, the endocrine system has to deal with “endocrine disruptors” that come from the external environment in the form of chemicals, such as pesticides and dioxins, found in our foods, our water, and the air we breathe.
Globally, it has been estimated that 20,000 people are killed yearly from direct exposure to pesticides; more than 500,000 illnesses yearly are due to pesticide use. Pesticide residues are found in air, soil, and water. They are found as well in most humans and animals. The majority of pesticides used are organophosphates and carbamate. They are used in schools, business offices, churches, apartment buildings, grocery stores, farms, and, homes on a regular basis.1
Pesticides in chronic low-dose exposure adversely affect the nervous system and cause cell-mediated immune deficiency, allergy, and autoimmunity. After symptoms occur in the immunological and neurological areas, problems in endocrine function may also occur. Chlorinated products, for example, act as weak estrogens and affect reproduction. These compounds have been associated with female infertility, miscarriages, and possible male infertility. Organophosphate (OP) pesticides have also been associated with male infertility with increased LH production (possibly secondary to testicular damage) and reduced numbers of morphologically healthy spermatozoa.2 Hexachlorocyclohexane (HCH) alters melatonin synthesis from the pineal gland and thus affects sleep. DDE (the breakdown product of DDT) can accumulate in the adrenal gland and cause atrophy.3 According to a study by the Environmental Protection Agency (EPA), 93% of autopsies conducted in 1982 indicated the presence of DDE. Organophosphates also seem to affect calcium metabolism. Agricultural workers exposed to OP pesticides have significantly decreased bone formation compared to healthy controls.4
North Americans accumulate harmful levels of dioxins in their bodies mostly through the ingestion of food. Some segments of the population, such as nursing babies and people who eat a diet high in animal fat or foods contaminated because of their proximity to dioxin release sites, are exposed to higher than average levels of dioxin. Dioxins accumulate in the fatty tissue in meat, fish, and dairy products. When people consume these foods, they also consume dioxins. The ingestion of dioxin in common foods has resulted in widespread low-level exposure in the general population. Others members of the population, such as Vietnam War veterans and some chemical plant workers, have accumulated additional dioxins because of their exposure to Agent Orange or other dioxin-contaminated chemicals in the workplace.
The World Health Organization (WHO) has studied the effect of abnormal levels of dioxin on the endocrine system, noting several serious disorders in animal and human studies.
Dioxin is not the only chemical that disrupts endocrine function. When the EPA measured the volatile organic compounds in adipose tissue of autopsies in the United States, a wide array of endocrine disruptors was discovered.
Exposure to chemicals has an impact on virtually every aspect of clinical endocrinology.
Selected Clinical Studies and Literature Reviews
To read more about exogenous endocrine disruptors, refer to the Selected Clinical Studies and Literature Review:
Paul Goettlich, Environmental Chemicals and Endocrinology, pp. 362.
Samuel S. Epstein, “Trade Secrets”: The Latest in a Long Line of Conspiracies Charges, pp. 366.
References
- Coburn T, Dumanosk D, Myers JP. Our Stolen Future.
Boston, MA: Little Brown, 1996. - Juhler RK, Larsen SB, Meyer O, et al. Human semen quality in relation to dietary pesticide exposure and organic diet. Arch Environ Cntam Toxic 1999;37:415-23.
- Chowdhury AR, Gautam AK, Venkatakrishna-Bhatt H. DDT (2,2 Bis9 p-Chlorphenyl)1,1,1-trichlorethaneinduced structural changes in adrenal glands of rats. Bull Environ Contam Toxic 1990;45:193-96.
- Compston JE, Vedi S, Stepen AB, et al. Reduced bone formation after exposure to organophosphates. The Lancet 1999;354:1791-92.
- Crinnion ND. Environmental medicine, Part 4: Pesticides — biologically persistent and ubiquitous toxins. Alternative Medicine Review 2000 Oct;5(5).